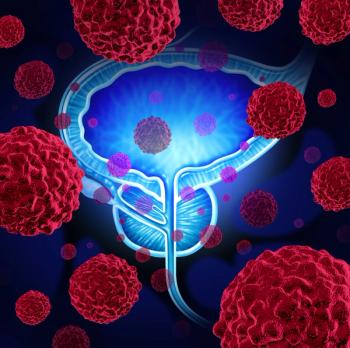
In Urothelial Cancer, Most Subtypes Benefit From Maintenance Bavencio (Avelumab), Faltas Says
A presentation at the 2021 American Society of Clinical Oncology meeting earlier this month reviewed recent findings from trials investigating the treatment of urothelial cancer.
Immunotherapy is transforming treatment of urothelial cancer, but there’s much work to be done in biomarker development to fill knowledge gaps and build better precision medicine approaches, according to
Faltas commented on three abstracts presented earlier this month during the 2021 Annual Meeting of the American Society of Clinical Oncology. Two were about trials that examined immunotherapy combinations in the neoadjuvant setting. The third concerned the use of Bavencio (avelumab) as maintenance therapy.
“So, what is the biological rationale for early systemic immunotherapy?” Faltas asked as his presentation began. He explained how surgery for primary and metastatic tumors in urothelial cancer is often not enough, because examinations of “micrometastatic clones” from within the same patient have shown how cancer has already spread by the time surgery occurs.
As Faltas explained, neoadjuvant cisplatin-based chemotherapy can improve overall survival, but some patients could benefit from additional therapy. Others are not eligible for cisplatin-based treatment.
Tecentriq (atezolizumab) with chemotherapy
First, Faltas reviewed results of a
The study met its primary end point, with, 27 of 39 patients (69%) achieving <pT2N0 at the time of radical cystectomy, including 44% who achieved pT0N0, which is considered a complete response rate.
Opdivo (nivolumab) and lirilumab
Combining two immunotherapy agents could be an option for patients not eligible for cisplatin therapy, but results from a phase 1b trial were disappointing. Patients who took neoadjuvant Opdivo (13 patients) or a combination of Opdivo and lirilumab (30 patients) tolerated the therapy well, by the complete response rates were low especially for Opdivo alone.
As Faltas explained more phase 3 trials involving neoadjuvant therapy are planned, for both cisplatin eligible and ineligible patients. For cisplatin-ineligible patients, combinations include trials with bempegaldesleukin — "bempeg" for short — and Opdivo or Keytruda (pembrolizumab) plus Padcev (enfortumab vedotin-ejfv). For cisplatin-eligible patients, combinations include an oral IDO inhibitor linrodostat with standard chemotherapy, with or without Opdivo. Other combinations involve Imfinzi (durvalumab) or Keytruda with the gemcitabine/cisplatin chemotherapy regimen.
Faltas outlined the biomarkers being studied to predict responses: tumor mutational burden, immune gene signatures, CDA density, TGF-beta signatures, among others.
However, overall, identifying a reliable clinical biomarker of response to immunotherapy has been elusive,” he said.
There are still many unanswered questions, said Faltas: “Are different immunotherapy combinations more effective than single agents in randomized controlled trials? Can we select patients who are likely to benefit form neoadjuvant immunotherapy based on a biomarker? And, finally, what is the best sequence of neoadjuvant, and maintenance lines of therapy?
Maintenance Bavencio
Faltas then moved to a post-hoc subgroup analysis of JAVELIN 100, a maintenance therapy study that has already resulted in an
The subgroup analysis involving the 700 patients who were randomized to Bavencio with best supportive care or best supportive care alone. An overall survival benefit was seen with Bavencio-based treatment across subgroups: upper- or lower-tract tumors, both metastatic or locally advanced, and unresectable disease prior to chemotherapy.
Those in the Bavencio group had prolonged survival compared with those in supportive care-only arm, especially among patients with upper tract tumors for whom survival improved from 17.4 months to 19.9 months. In patients with lower-tract disease, survival improved from 14.1 months to 22.5 months; and in the metastatic disease arm, survival increased 14.1 months vs. 18.2 months.
"We can see that the clinical benefit of maintenance avelumab is consistent across the majority of these subgroups," Faltas said.
"My interpretation of this data is that maintenance avelumab should be offered to all patients who would qualify," he continued.
Patients with the luminal molecular subtype may not derive as much benefit, although, the confidence intervals are wide, making the finding hard to interpret, he noted/
Faltas then reviewed data from several studies showing the challenges that remain in developing biomarkers in UC, in part because biomarkers can evolve in a given cancer over time.
“I suggest that the relationship between molecular subtypes in response to immunotherapy should be viewed as a continuum,” he said.
Neuroendocrine tumors are rare but are “exceptionally responsive to immunotherapy,” and basal tumors also likely see a high degree of benefit from immunotherapy, observed Faltas. Other subtypes may be less responsive or even resistant to immunotherapy.
“In order to leverage this understanding to develop a clinical biomarker, we need a single sample classifier,” he said, showing an example of one such tool. But even the way molecular subtypes are named doesn’t speak to the way different cell components function when it comes to the way they behave in cancer.
Newsletter
Get the latest industry news, event updates, and more from Managed healthcare Executive.