Smart Insulins and a Combined Insulin/Glucagon Receive Research Awards
The Type 1 Diabetes Grand Challenge has provided awards to six universities —including three in the United States — to fund research of novel therapies to treat patients with type 1 diabetes.
The Type 1 Diabetes Grand Challenge has awarded £2.7 million (about $3.6 million) to six different projects aimed at developing novel insulins to treat patients with type 1 diabetes. The universities in the United States, Australia, and China that received the awards aim to design insulins that act faster and more precisely. The Type 1 Diabetes Grand Challenge is a partnership between the Steve Morgan Foundation, Diabetes UK and JDRF.
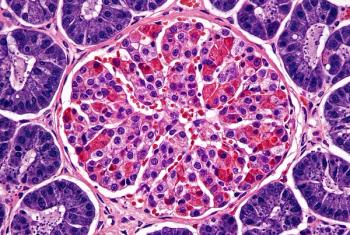
Type 1 diabetes is an autoimmune disease that affects about 2 million Americans, about 5% to 10% of all diabetes cases, according to the Centers for Disease Control and Prevention (CDC). In type 1 diabetes, the pancreas does not make insulin.
“Even with the currently available modern insulins, people living with type 1 diabetes have to put lots of effort into managing their diabetes every day to find a good balance between acceptable glycemic control on the one hand and avoiding hypoglycemia on the other. The funded six new research projects address major shortcomings in insulin therapy,” Tim Heise, vice chair of our Novel Insulins Scientific Advisory Panel, said in a
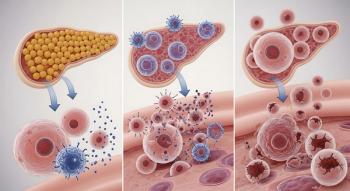
One project that received an award is focused on designing a protein that combines insulin with another hormone, glucagon. Unlike insulin, which helps remove glucose from the blood, glucagon stimulates the liver to release more glucose when levels in the blood run low. Having both hormones included in one formulation could keep blood glucose levels stable by working to prevent high and low blood glucose levels.
This research on combining insulin with glucagon is being conducted by Michael A. Weiss, M.D., Ph.D., and his team at Indiana University, along with Raimund Herzog, M.D., and colleagues at Yale School of Medicine. The one-year award for $480,000 will be shared between Indiana University and Yale.
Weiss, who is chair of the department of Biochemistry & Molecular Biology at Indiana University, will conduct studies in rats with type 1 diabetes how stable the dual hormone molecule. They will also explore different ways to manufacture the insulin-glucagon molecule.
“We hope to advance to clinical trials an ultra-stable polypeptide bihormonal therapy that would provide once-a-day or once-a-week basal insulin therapy with reduced risk of hypoglycemia relative to current insulin-only products,” Weiss told Managed Healthcare Executive. “We next will seek a rapid-acting fusion protein for use in an insulin pump and in closed loop systems to enhance time in range.”
The next step for the Indiana University/Yale teams is to optimize the insulin-glucagon fusion protein to obtain the most effective ratio of hormonal activities and enable low-cost manufacturability.
Four of the Grand Challenge projects involve scientists creating and testing novel insulin formulations that can respond to changing blood glucose levels, known as glucose responsive insulins (GRIs) or “smart insulins.”
“Glucose-responsive (so-called ‘smart’) insulins are regarded as the holy grail of insulin as they would come as close to a cure for type 1 diabetes as any drug therapy could,” Heise said.
One smart insulin project is being conducted at Wayne State University. This group was awarded £417,503 ($551,847) by the Type 1 Diabetes Grand Challenge. Zhiqiang Cao, Ph.D., professor, Chemical Engineering and Materials Science, and his team have developed a glucose-responsive insulin is more sensitive to changing glucose levels.
Cao told Managed Healthcare Executive “the award will allow us to finalize the smart insulin formulation and develop strategies for manufacturing and regulatory approval for clinical trials. Our ultimate goal is a smart insulin product, and we anticipate advancing to clinical trials in the next two to three years at the earliest.”
Another project focused on a smart insulin is being conducted by researchers at Notre Dame. In this project, Professor Matthew Webber, Ph.D., associate professor of Chemical and Biomolecular Engineering, and his team have developed a smart insulin delivery system that uses tiny particles called nanocomplexes, which contain insulin. These nanocomplexes can be injected under the skin to create a reservoir of insulin. If glucose levels in the blood rise, insulin is automatically released from the stored particles.
The team has shown that in pigs with type 1 diabetes, a single injection of the insulin nanocomplexes is enough to keep glucose levels stable for a week.
Webber and his colleagues will continue their research with pigs and explore ways to manufacture the insulin-containing nanocomplexes to allow them to be stored at room temperature. Researchers are collaborating with and unnamed nonprofit company for the development of this product.
The final project to receive the Type 1 Diabetes Grand Challenge is working to develope an ultrafast, short-acting insulin. Even with the fastest insulins that are currently available, there is still a delay between the drug being administered and the point it starts to act on glucose in the blood.
Newsletter
Get the latest industry news, event updates, and more from Managed healthcare Executive.