Review Finds Lower Relapse Rates After Menopause But Increased Disability in Women with MS
The reduced relapse rate among postmenopausal women could be due to diminished immune system activity, according to the authors.
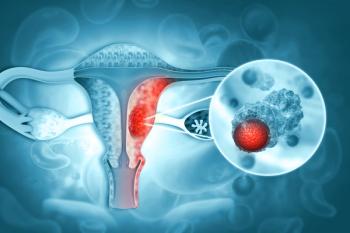
Multiple sclerosis (MS) is about three times more prevalent in women than men, and hormonal differences are believed to be the culprit. Research suggests
After menopause, a shift in hormone balance leads to a decrease in blood estrogen levels, which may affect MS disease progression. Zahra Shahraki, associate professor at the Zabol University of Medical Sciences in Iran, and her colleagues conducted a systematic review and meta-analysis to gauge the effect of menopause on relapse rate and disability status in patients with MS. Their results were published earlier this month in the journal
After searching several databases, the researchers included four studies published between 2017 and 2020. Each study enrolled between 37 and 148 patients with a mean age range between 47 and 50 years. Two studies took place in Italy, one in Portugal, and one in Spain.
Results showed that the mean annual relapse rate significantly decreased after menopause compared to premenopausal time. However, mean disability scores measured with the Expanded Disability Status Scale (EDSS) significantly increased post menopause versus pre-menopause. Premenopausal EDSS scores ranged from 1.5 to 2, indicating patients had no disability with minimal symptoms or minimal disability. After menopause, mean EDSS scores ranged from 2 to 3.1, signifying moderate disability.
The authors note that postmenopausal reduced relapse rates could be due to decreased immune system activity, and reduced neuroprotection due to decreased estrogen levels may contribute to the increased disability levels.
They wrote, “It is evident that the anti-inflammatory role of [estrogens] after menopause decreases, which leads to aggressive, inflammatory damage of axons plus myelin sheets, as well as disability progression.”
Newsletter
Get the latest industry news, event updates, and more from Managed healthcare Executive.