Researchers Link Specific Protein to Diabetic Cardiomyopathy
New research suggests that activation of the PPARδ protein, which is linked to inflammation, could treat or prevent diabetic cardiomyopathy, a serious heart condition.
Researchers at the University of Barcelona in Spain have identified a potential target for treating patients with diabetes who have developed a serious heart condition called diabetic cardiomyopathy.
In people with cardiomyopathy, the heart has a hard time pumping blood to the rest of the body, and this can cause chest pain, shortness of breath, swelling, fatigue, dizziness and fainting. It can lead to heart failure, blood clots, heart valve problems and cardiac arrest.
People with diabetes have a higher chance of developing cardiomyopathy. High blood sugar levels from diabetes can damage the blood vessels, making them more likely to develop fatty deposits. One study
In the University of Barcelona study, which was
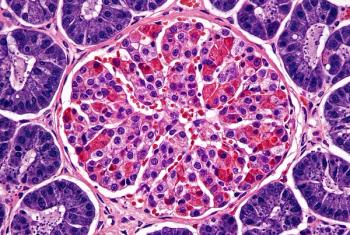
Researchers found that the PPARδ protein is linked to metabolic diseases marked by inflammation, including insulin resistance induced by obesity or diabetes, dyslipidemia or metabolic fatty liver disease. They found that activating the PPARδ receptor can help to slow down the processes of inflammation and fibrosis in both animal models and human cardiac cells under hyperglycemic conditions.
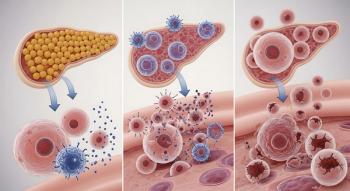
In diabetes or obesity, insulin resistance can cause the heart to derive energy almost exclusively from mitochondrial oxidation of fatty acids. This causes lipid accumulation in the myocardium and leads to lipotoxicity, which results in the heart muscle demanding more oxygen.
Diabetic hyperglycemia and lipotoxicity trigger cardiac inflammation and fibrosis through the activation of proinflammatory and profibrotic transcription factors (NF-қB and AP-1). Once activated, these factors drive the process of cardiac remodeling, which increases myocardial stiffness and impairs cardiac relaxation after contraction.
The activation of NF-қB and AP-1, together with mitogen-activated protein kinase (MAPK) activity, induces cardiomyocyte cell death, which also contributes to contractile dysfunction in diabetic cardiomyopathy.
“Together, all these processes lead to extracellular cardiac remodeling, contractile dysfunction, left ventricular hypertrophy and dilated cardiomyopathy, ultimately leading to heart failure,” Xavier Palomer
, one of the researchers involved in the study, said in a news release. Palomer, along with Manuel Vázquez-Carrera led the study. Both are from the University of Barcelona’s Faculty of Pharmacy and Food Sciences, the University of Barcelona Institute of Biomedicine and the Sant Joan de Déu Research Institute.
“Inhibition of these MAPKs can prevent inflammation and fibrosis not only in the heart, but also in other organs and tissues such as the liver, lung, kidney or even skeletal muscle, in various pathological conditions,” Vázquez-Carrera said.
A therapy that targets PPARδ was granted accelerated approval in August 2024 by the FDA to treat patients with primary biliary cholangitis (PBC), a progressive autoimmune disease that results from the destruction of the bile ducts in the liver. Gilead’s Livdelzi (seladelpar) is an oral therapy that activates PPARδ and is able to reduce bile acid.
Newsletter
Get the latest industry news, event updates, and more from Managed healthcare Executive.