Patients with Type 1 Diabetes Have Higher Risk of Epilepsy
Findings from observational studies in the past have not been consistent on the link between type 1 diabetes and epilepsy.
A new meta-analysis has showed that people with type 1 diabetes have a higher incidence of epilepsy, and this association was consistent in children and adults, according to a study
Type 1 diabetes is an autoimmune disease that affects about 2 million Americans, about 5% to 10% of all diabetes cases, according to the Centers for Disease Control and Prevention (CDC). In type 1 diabetes, the pancreas does not make insulin.
Researchers at the department of Neurology at the Liaocheng People’s Hospital in China noted that patients with type 1 diabetes are susceptible to neurological disorders, including epilepsy. They noted that findings from observational studies in the past have not been consistent.
Researchers conducted a search of PubMed, Embase, and Web of Science for studies of type 1 diabetes or epilepsy up through Aug. 15, 2023. They included in their meta‐analysis six observational studies with 10 datasets that in total included more than 8 million patients. Among them, 100,414 patients had type 1 diabetes.
Researchers found that during a follow‐up duration of between 5.4 and 15.2 years, 98,644 cases (1.23%) of epilepsy were observed. Compared with participants with normal glycemic levels, those with type 1 diabetes were shown to have a higher incidence of epilepsy, after adjustment of potential confounding variables including age and sex.
Researchers noted a previous meta-analysis published in 2017 that include three observational studies, but they wrote that sensitivity and subgroup analysis were not performed because of the limited study.
In the current analysis, the sample size was larger and included studies that included longitudinal follow‐ups. The Liaocheng People’s Hospital researchers said this enables a potential relationship between type 1 diabetes and the incidence of epilepsy to be assessed.
“Multivariate analyses were performed in all of the included studies when the association between type 1 diabetes and the incidence of epilepsy was evaluated, which suggested that the association was not likely to be confounded by factors such as age, sex, or history of brain injury,” they wrote.
Researchers also conducted sensitivity and subgroup analyses. This subgroup analysis, the Liaocheng People’s Hospital researchers said, that the relationship between type 1 diabetes and an increased risk of epilepsy may be stronger in short‐term studies of less than 10 years compared with long‐term studies of more than 10 years.
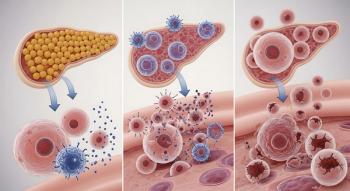
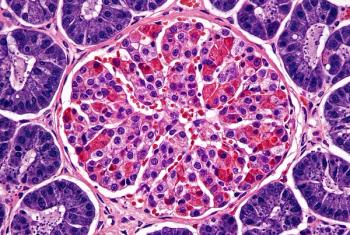
But the mechanism of the relationship between type 1 diabetes and epilepsy is not known, they say. One mechanism could be autoimmune antibodies, particularly glutamic acid decarboxylase (GAD), a marker of insulin-related diabetes. Several studies in small patient populations have a found a connection between GAD antibodies and some forms of epilepsy.
In one study
The Liaocheng People’s Hospital researchers said their results would need to be validated with prospective studies to determine the underlying mechanisms and to explore whether optimizing glycemic control could reduce the risk of epilepsy in patients with type 1 diabetes.
One limitation, they said, was that database codes, rather than clinical diagnosis, were used to determine diagnosis of type 1 diabetes and epilepsy. An additional limitation is that most the datasets used included children. “The results of the meta‐analysis were primarily driven by studies including children with type 1 diabetes, while only one dataset including older people with type 1 diabetes.”
Newsletter
Get the latest industry news, event updates, and more from Managed healthcare Executive.