Immunotherapy vs. Chemotherapy as Second-line Treatment for NSCLC
A real-world evidence study shows an advantage in median overall survival among non-small cell lung cancer patients who were treated with second-line immunotherapy compared to those treated with chemotherapy. Multivariable analysis showed healthcare resource utilization was comparable.
In a real-world retrospective study of veterans with advanced non-small cell lung cancer (NSCLC), second-line immunotherapy led to significantly better survival rates than did second-line chemotherapy. The
Median overall survival was 8.7 months in the immunotherapy group compared with 7 months in the chemotherapy group. Black patients, often underrepresented in clinical trials, had better outcomes than whites. Shorter survival times were associated with immunotherapy as first-line therapy, treatment with radiation and squamous cell histology.
Williams and her colleagues also looked at healthcare resource utilization, noting that there has been little research in this area because researchers have tended to focus on survival and other clinical outcomes. In their study, patients treated with second-line immunotherapy had an average of 47 outpatient visits and 14 oncology-specific outpatient visit. The chemotherapy patients had fewer visits: 31 outpatient visitsand nine oncology-specific ones. The proportion of hospitalizations was similar: 49% of immunotherapy patients had a hospitalization compared with 42% of chemotherapy patients. However, after a multivariable analysis, the differences in healthcare resource utilization disappeared and immunotherapy and chemotherapy groups were about the same.
The side effects were similar with those found in other real-world studies of second-line NSCLC therapy. The most common were dyspnea, colitis/enterocolitis, and anemia in the immunotherapy group and anemia, colitis/enterocolitis, and nausea/vomiting in the chemotherapy group. Roughly 18% of the immunotherapy group had no side effects, compared with 30% of the chemotherapy group.
The researchers did not adjust for duration of drug exposure but said the “surprising” findings on post-treatment healthcare resource utilization and side effects may relate to treatment duration and pre-existing side effects.
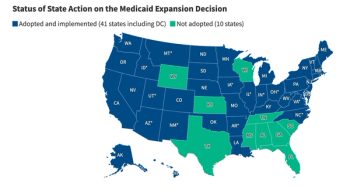
Patients were more likely to receive immunotherapy in the latter years studied, suggesting a trend in clinical practice. The researchers also found geographic differences. Immunotherapy was used more often in the West and Midwest.
Patients who received immunotherapy as first-line treatment were significantly less likely to receive it as second-line treatment, according to Williams and her colleagues. They found, though, that older patients, in particular those with high comorbidity scores, were more likely to be treated with second-line immunotherapy. That finding, they say, may indicate that healthcare providers recommend immunotherapy over chemotherapy in patients who are perceived to be more frail, likely, in part, because they are concerned that older, less healthy patients might not be able to tolerate the side effects of chemotherapy.
Real-world studies are crucial to understanding the medical and economic consequences of immunotherapies and to identify unmet needs, wrote Williams and colleague. Clinical trials tend to be highly selective, they noted. Participants tend to be relatively young and healthy. in contrast to the mostly elderly general population of patient with metastatic NSCLC seen in general oncology practice. They point out that “approximately 70% of patients with NSCLC would fail to meet the inclusion criteria for the clinical trials used to approve these treatments.”
Newsletter
Get the latest industry news, event updates, and more from Managed healthcare Executive.