FDA approves Roctavian, the First Gene Therapy for Hemophilia A
The price tag of $2.9 million is typical of a new wave of gene therapies. The manufacturer, BioMarin Pharmaceutical, is offering arrangements that will link the price paid by payers to how well patients respond to the treatment.
The FDA approved Roctavian (valocotogene roxaparvovec) today. It is the first gene therapy for hemophilia A, the most common form of the disease.
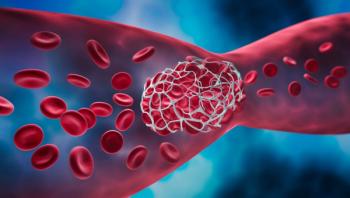
The therapy’s maker, BioMarin Pharmaceutical, is pricing the therapy at $2.9 million for a one-time treatment. The gaudy price tag is striking, but multimillion dollar prices for the growing number of gene therapies are common. The manufacturers and independent cost-effectiveness research groups say the seven-figure prices are justified, in part because patients will avoid the costs of lifelong treatments with other therapies. Hemophilia A is a hereditary disorder caused by a lack of blood clotting factor VIII, and patients with severe cases receive frequent infusions of clotting factors.
There are lingering questions, though, about how “durable” the supposedly one-time gene therapies are and whether patients will need eventually need to resume infusions of clotting factors or be treated in other ways. Payers, academic and cost-effectiveness experts have suggested that insurers tie payment for the gene therapies to measurable outcomes, which in the case of hemophilia might be how long the patient doesn’t need clotting factor infusions.
BioMarin is setting up an outcomes program for Roctavian that will reimburse payers up to 100% of cost if person does not respond to treatment. Part of the cost will be reimbursed on prorated basis if the patient stops responding after the first four years.
The FDA approved Hemgenix (etranacogene dezaparvovec), another gene therapy for hemophilia, in November 2022, and its manufacturer, CSL Behring in suburban Philadelphia, priced it at $3.5 million. The company
Pfizer issued a
Related:
The FDA approval of Roctavian was expected, although path thorough the FDA approval process has been long and tortuous and included a 2020
The agency’s approval is based on results of the BioMarin-sponsored Gene8-1study, an open-label study that included 134 participants who received a Roctavian solution. The
Newsletter
Get the latest industry news, event updates, and more from Managed healthcare Executive.