Alcohol and A-fib Risk: Best To Lay Off the Booze
Animal, human and epidemiologic studies point to an association between alcohol consumption and atrial fibrillation. The association is especially strong with binge drinking.
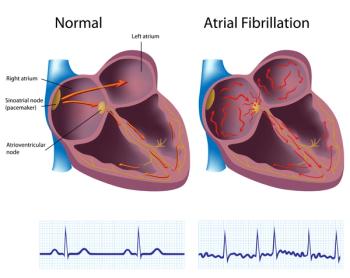
Atrial fibrillation (A-fib) is a widespread disease whose incidence is expected to increase more than 60% by 2050. It is much more prevalent in older adults, although observational studies suggest a strongly dose-dependent relationship between A-fib incidence and alcohol consumption.
Authors of a review of studies of alcohol and A-fib concluded that emphasizing alcohol consumption is a modifiable risk factor is the most effective means of combating A-fib.
“Abstinence from alcohol consumption or reduction in alcohol intake is consistently shown to be the most effective method to reverse the cardiac effects of excessive alcohol consumption,” wrote
The authors said abstinence from alcohol consumption has been associated with a 20% reduced risk of A-fib, although they noted light alcohol use has been associated with some cardioprotective benefits, including reduced risk of myocardial infarction.
In mouse models, chronic alcohol consumption increased A-fib susceptibility up to 95.2%. That research as well as studies of people, have shown that the heart’s electrical functioning is profoundly affected by drinking patterns. In one human, placebo-controlled trial referenced by the authors of the Cardiology in Review paper, acute alcohol exposure significantly shortened effective refractory periods (ERP), which the heart chamber requires to refill with blood prior to the next contraction.
“Through potential shortening of the atrial ERP (effective refractory periods) , alcohol consumption is shown to be associated to A-fib even in younger patients,” Kaul and his fellow authors wrote.
The effects of alcohol on the autonomic nervous system have been widely studied. The autonomic nervous system regulates speed of heart rate via the parasympathetic and sympathetic nervous systems, and these functions are disrupted by heavy drinking.
Alcohol also stimulates the production of adrenaline, and “binge drinking has been shown to induce a 24-hour hyperadrenergic state...hence promoting atrial arrhythmias,” the authors wrote. The Centers for Disease Control and Prevention defines binge drinking as five or more drinks on one occasion for men and four for women/
Chronic alcohol consumption also leads to atrial structural malformation through increased oxidative stress, mitochondrial dysfunction and abnormal fatty acid metabolism, they noted.
“A 2015 study showed a correlation between A-fib, alcohol consumption, and the presence of increasing atrial fibrosis, a sign of adverse remodeling,” the authors noted
In one study, the risk of A-FIB was 3.2 times higher for binge drinkers compared with light drinkers. The authors noted that although habitual alcohol consumption is a risk factor for A-fib, an individual episode of binge drinking also may trigger A-fib.
However, the association with A-fib is strongest for habitual drinkers, based on a large cohort study of 9.8 million in which 195,829 participants developed new onset A-FIB. The investigators reported a 2% increased risk of A-fib per gram of alcohol ingested over a weekly period.
Kaul and his review team also looked at the relationship of drinking and A-fib to comorbidities. They noted heavy drinking may lead to obesity, a known risk factor for A-fib. “The obesity epidemic almost seems to coincide with the onset of the A-fib epidemic,” they wrote.
“Researchers have demonstrated that long-term, sustained weight loss of more than 10% results in a reduction in A-fib or burden through a six times greater probability of arrhythmia-free survival when compared to groups associated with a weight loss of 3% to 9%,” they wrote.
Newsletter
Get the latest industry news, event updates, and more from Managed healthcare Executive.