- MHE September 2022
- Volume 32
- Issue 9
Gene Therapies for Hemophilia. Possibly Curative, Likely Ultraexpensive
Three gene therapies in late-stage development are designed to supply working copies of genes that people with hemophilia are missing. They may be one-time, curative treatments, but the seven-figure price tags will be an issue.
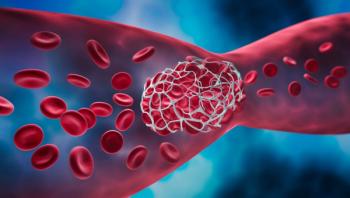
Hemophilia is a rare, X-linked, hereditary bleeding disorder characterized by blood clotting factor deficiencies that affects mainly males. It results in excessive bleeding, particularly in the joints, soft tissues and muscles. The bleeding usually happens after internal or external trauma, but in rare cases, it occurs spontaneously. According to the CDC, up to 33,000 males in the United States live with hemophilia, but the condition can be fatal. Hemophilia is divided into subtypes, the two most common of which are hemophilia A and hemophilia B. In hemophilia A, blood coagulation factor VIII is deficient; in hemophilia B, it’s factor IX.
Blood coagulation occurs through two series of cascading events: the intrinsic and the extrinsic pathways. The two work simultaneously, activating various coagulation factors, which are proteins in the blood and are part of the intricate, multistep process that stanches bleeding. Ultimately the intrinsic and extrinsic pathways merge into a common pathway to form thrombin. Thrombin helps form fibrin, which is integral in blood clot formation. Without factor VIII or factor IX, the intrinsic pathway cannot be activated and blood coagulation cannot occur.
Until recently, hemophilia treatment goals have focused on prophylaxis by temporarily replacing deficient clotting factors. This involves lifelong intravenous infusions of factor concentrate that, although effective in preventing life-threatening bleeding and preserving joint function, place a heavy burden on patients and their families. Infusions can be painful and inconvenient and, over time, cause damage to veins. Moreover, people can develop inhibitors to the replacement factors, which eventually diminishes their effectiveness.
Research over the past several decades has focused on finding therapies that would go beyond replacement factors and perhaps allow people living with hemophilia to lead lives as normal as those without the disease. Many novel treatments are under development for hemophilia A and B, but this article will focus primarily on hemophilia B treatments.
Gene therapy
Research on gene therapy looks promising with regard to significantly improving the quality of life in people living with hemophilia. With gene therapy, an adeno-associated virus (AAV) vector ferries DNA into the patient’s cells that carries the instructions for producing the deficient clotting factor. Hepatocytes produce most clotting factors, so they are the target cells for hemophilia gene therapy. Even a small increase in clotting factor levels can convert a severe case of hemophilia into a mild one.
Several gene therapy candidates are currently in late-stage clinical trials. At least three are for hemophilia B. They are intended to be one-time treatments and possibly curative. The excitement about these gene therapies that could be curative is tempered by their price, which is likely to be in the millions of dollars for a single treatment. If the price tags are as high as expected, they would rank as the world’s most expensive treatments. The drug developers say seven-figure price tags are justified by development costs and the avoidance of lifelong treatment that winds up costing in the millions of dollars. Some payers are selling special coverage for these and other extraordinarily high-priced therapies.
Currently, the leading gene therapy candidate is one that has been developed by uniQure, headquartered in Amsterdam, and CSL Behring, in suburban Philadelphia. They have partnered to develop EtranaDez (etranacogene dezaparvovec), which uses a vector called AAV5 to deliver the Padua gene variant of factor IX (FIX-Padua). FIX-Padua generates factor IX proteins that are potentially five to eight times more active than the factors the body normally produces. Moreover, the AAV5 may be effective in most hemophilia B patients who have developed antibodies to other AAV vectors.
The phase 3 HOPE-B pivotal clinical trial demonstrated that EtranaDez is more effective than standard factor IX prophylactic therapy in reducing annualized bleeding rate. The trial enrolled 54 adult males with moderate to severe hemophilia B. All participants received a single intravenous infusion of the study treatment after receiving standard factor IX prophylaxis. Participants maintained stable factor IX levels and activity at 18 months following one infusion, and an impressive 98% of patients were able to discontinue prophylactic factor IX treatment. Additionally, study data showed that EtranaDez is effective in patients with viral vector antibodies.
These results were presented in February at the European Association of Haemophilia and Allied Disorders 2022 annual meeting. In May 2022, the FDA accepted the biologics license application (BLA) for EtranaDez for priority review based on those results. Priority review of a BLA is granted to treatments that would significantly improve the safety or efficacy of the current treatment, diagnosis or prevention of serious conditions.
Close on EtranaDez’s heels is Pfizer’s fidanacogene elaparvovec. Like EtranaDez, Pfizer’s gene therapy for hemophilia B uses an AAV vector to deliver the FIX-Padua variant. Following encouraging results from phase 1 and 2 studies, Pfizer has initiated the BENEGENE-2 phase 3 trial to evaluate the safety and efficacy of fidanacogene elaparvovec in adult males with moderate to severe hemophilia B. The study enrolled 45 men aged 18 to 65 years with moderate to severe hemophilia. The participants will receive a single intravenous infusion of fidanacogene elaparvovec after receiving a minimum of six months of factor IX prophylaxis therapy and will be evaluated over six years. The study’s primary outcome is the annualized bleeding rate. Primary results are expected in November 2022.
Freeline Therapeutics, a clinical-stage biotechnology company based in the U.K., is taking a slightly different approach toward hemophilia B gene therapy. Its FIX-Padua delivery vehicle is a synthetic AAV capsid (AAVS3) designed to convert more target liver cells than other vectors, such as AAV5.
The company has completed the B-AMAZE phase 1 and 2 study of its investigational treatment, verbrinacogene setparvovec, for use in adult males with moderate to severe hemophilia B. In the B-AMAZE study, 10 adult males with moderate to severe hemophilia B received one of four treatment doses. All participants received prophylactic immunosuppression of prednisolone with or without tacrolimus. Primary outcomes were safety and efficacy as assessed by factor IX levels at 26 weeks. All but one of the participants had sustained factor IX activity at the 27-month median follow-up. Additionally, patients had fewer bleeding episodes and reduced use of factor IX therapy compared with baseline. Researchers conclude that low doses of verbrinacogene setparvovec can achieve normal factor IX levels in patients with moderate to severe hemophilia B. After a successful meeting after its phase 2 trial, Freeline Therapeutics plans to proceed with a phase 3 trial.
Rosanna Sutherby, Pharm.D., is an independent medical writer and community pharmacist in High Point, North Carolina.
Articles in this issue
Newsletter
Get the latest industry news, event updates, and more from Managed healthcare Executive.